
Table of Contents
Cortisol is a steroid hormone the adrenal glands produce in response to stress. It plays a vital role in the body's stress response system, regulating metabolism, blood sugar levels, immune function, and cardiovascular function.
Key Takeaways
- Definition: Cortisol is a steroid hormone produced by the adrenal glands, often referred to as the "stress hormone."
- Function: It helps regulate metabolism, blood sugar levels, and immune response during stress.
- Imbalance: High cortisol levels can lead to issues like weight gain, anxiety, and high blood pressure, while low levels can cause fatigue and weakness.
- Circadian Rhythm: Cortisol levels naturally fluctuate throughout the day, peaking in the morning.
- Stress Response: Chronic stress can lead to consistently high cortisol levels, impacting overall health.
- Management: Techniques like relaxation, exercise, and proper sleep can help manage cortisol levels.
Cortisol Explained
Cortisol, or the stress hormone, is an essential steroid hormone in the glucocorticoid class of hormones that affects almost every organ in the body.
The vital hormone regulates stress response, metabolism, immune function, cardiovascular regulation, and central nervous system modulation.
Its intricate role in the body's physiology underscores the importance of maintaining a healthy balance of cortisol levels for optimal health and well-being.
Cortisol Production And Regulation
Production In Adrenal Glands
Cortisol is primarily produced and secreted by the outer layer of the adrenal cortex, known as the zona fasciculata.
The zona fasciculatais the largest region of the adrenal glands, which are small triangular-shaped glands on top of the kidneys.
Cortisol production follows a diurnal rhythm, with levels highest in the morning and gradually declining throughout the day.
Biosynthesis And Metabolism
The process of cortisol biosynthesis involves several enzymatic reactions and is regulated by a complex cascade of signaling molecules.
The production of cortisol begins with the uptake of cholesterol into the adrenal cortex cells. Cholesterol is the precursor molecule for cortisol synthesis. It is obtained from circulating lipoproteins or synthesized within the adrenal gland itself.
Once inside the adrenal cortex cells, cholesterol undergoes a series of enzymatic conversions. The rate-limiting step in cortisol synthesis is the conversion of cholesterol to pregnenolone, which is catalyzed by the enzyme cholesterol side-chain cleavage enzyme, also known as P450scc.
Pregnenolone then undergoes a series of enzymatic reactions in the endoplasmic reticulum of the adrenal cortex cells to form cortisol.
These reactions involve the action of several enzymes, including 3β-hydroxysteroid dehydrogenase (3β-HSD), 17α-hydroxylase, 21-hydroxylase, 11β-hydroxylase, and 17β-hydroxysteroid dehydrogenase (17β-HSD).
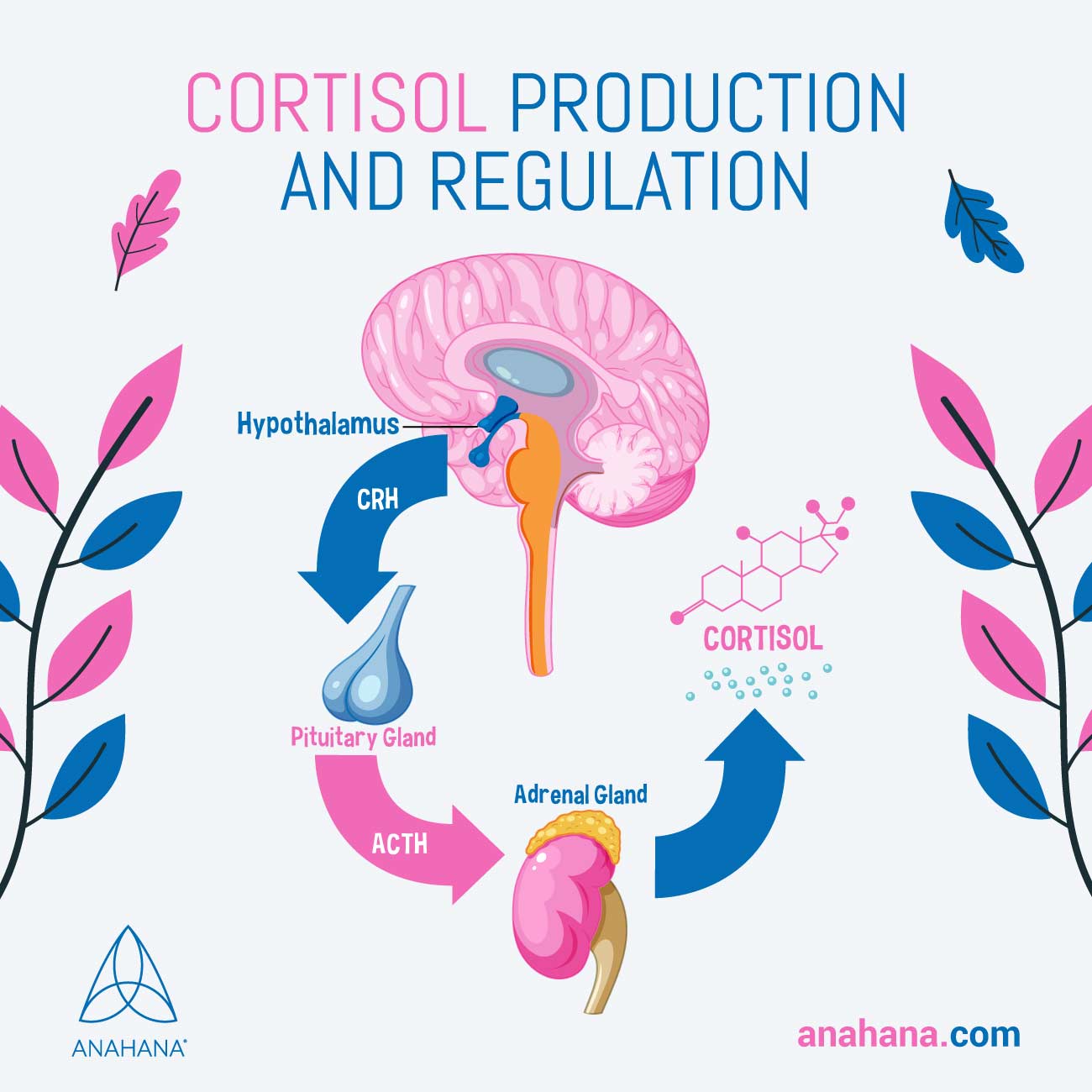
Regulation by the Hypothalamic-Pituitary-Adrenal (HPA) axis
The production of cortisol is regulated by the hypothalamic-pituitary-adrenal (HPA) axis.
The hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the anterior pituitary gland to secrete adrenocorticotropic hormone (ACTH).
ACTH then binds to specific receptors on the adrenal cortex cells, activating signaling pathways that increase the production and release of cortisol.
Feedback Mechanisms
The regulation of cortisol production also involves a feedback mechanism. Cortisol inhibits the secretion of CRH from the hypothalamus by directly acting on CRH-releasing neurons. It reduces the synthesis and release of CRH, leading to a decrease in its availability for stimulating the pituitary gland.
At the pituitary gland level, cortisol suppresses the secretion of ACTH through negative feedback.
Cortisol binds to specific receptors on corticotroph cells in the anterior pituitary gland, inhibiting the synthesis and release of ACTH. This reduces the stimulation of the adrenal glands, resulting in decreased cortisol production.
The negative feedback system is finely tuned to maintain cortisol levels within a narrow range.
When cortisol levels drop below the normal range, the reduced negative feedback allows for increased release of CRH and ACTH. This stimulates the adrenal glands to produce and release more cortisol, restoring cortisol levels to the optimal range.
Effects Of Cortisol On The Body
Stress Response And The "Fight Or Flight" Reaction
The stress response, or the "fight or flight" reaction, is a fundamental survival mechanism that helps individuals respond to perceived threats or challenges.
Cortisol plays a central role in orchestrating this physiological response that happens in several steps:
- Stressful stimuli: When the brain perceives a stressful situation, the hypothalamus, a region in the brain, releases CRH.
- Prompting secretion: CRH stimulates the pituitary gland to secrete ACTH.
- Adrenal glands release cortisol: ACTH, in turn, triggers the adrenal glands, specifically the adrenal cortex, to release cortisol into the bloodstream.
- Hormones: Cortisol and other stress hormones like adrenaline and norepinephrine prepare the body for action.
- Increase in blood flow: It increases heart rate and blood pressure, enhances blood flow to the muscles and brain, and diverts energy from non-essential functions like digestion and reproduction.
- Necessary physiological changes: These physiological changes help individuals confront the threat head-on or escape.
Metabolism And Blood Sugar Regulation
Cortisol plays a crucial role in regulating metabolism and blood sugar levels.
- Breaks down nutrients: It mobilizes energy stores during stress by increasing the breakdown of proteins, fats, and carbohydrates.
- Makes glucose: Cortisol stimulates gluconeogenesis, synthesizing glucose from non-carbohydrate sources, such as amino acids and glycerol. This leads to elevated blood sugar levels, ensuring an adequate energy supply to meet the body's demands during stressful situations.
- Regulates insulin: Cortisol inhibits insulin activity, reducing glucose uptake by peripheral tissues.
These metabolic effects of cortisol help provide the body with the necessary fuel to cope with stress but can contribute to insulin resistance and metabolic imbalances when cortisol levels are chronically elevated.
Immune System Modulation
Cortisol exerts potent immunosuppressive and anti-inflammatory effects. It inhibits the production of pro-inflammatory cytokines, such as interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-alpha), and reduces the activity of immune cells, including lymphocytes and macrophages.
While these actions help prevent excessive inflammation and immune responses, prolonged elevation of cortisol levels can impair immune function.
Chronic stress and high cortisol levels can lead to immune system dysregulation, making individuals more susceptible to infections, impairing wound healing, and contributing to autoimmune disorders.
Cardiovascular Effects
Cortisol influences cardiovascular function through various mechanisms. It increases blood pressure by promoting vasoconstriction, narrowing the blood vessels.
Cortisol also enhances the responsiveness of blood vessels to other vasoconstrictive substances, such as adrenaline and angiotensin II. The renin-angiotensin-aldosterone system, regulating blood volume and pressure, is also impacted
Chronic elevation of cortisol levels can contribute to hypertension, atherosclerosis, and an increased risk of cardiovascular diseases.
Moreover, cortisol influences body fat distribution, favoring fat deposition in the abdominal region, which is associated with an increased risk of cardiovascular problems.
Central Nervous System Effects
Cortisol significantly affects the central nervous system, influencing mood, cognition, and the sleep-wake cycle. High cortisol levels can contribute to anxiety, irritability, and even depression.
Cortisol receptors, including emotional regulation and cognitive function regions, are widely distributed in the brain.
Prolonged exposure to elevated cortisol levels can lead to impaired memory, decreased attention, and difficulties with learning and decision-making. Cortisol also plays a role in the regulation of the sleep-wake cycle.
Elevated cortisol levels in the morning promote wakefulness and alertness, while lower levels at night contribute to the initiation and maintenance of sleep.
Disruptions in cortisol patterns, such as in conditions like insomnia or certain sleep disorders, can adversely affect sleep quality and overall neurological functioning.
Cortisol And Stress
Effects Of Chronic Stress On Cortisol Levels
Chronic stress, characterized by prolonged and repeated exposure to stressors, can lead to dysregulation of the HPA axis. In cases of chronic stress, cortisol levels may become chronically elevated.
This can have detrimental effects on various systems in the body. Prolonged exposure to high cortisol levels can lead to:
- Disruptions in immune function
- Metabolic imbalances
- Cognitive impairments
- Mood disorders
- Increased susceptibility to diseases.
Acute Vs. Chronic Stress Responses
The body's response to acute stress, such as a sudden threat or a challenging short-term situation, is characterized by a temporary increase in cortisol levels. This adaptive acute stress response helps individuals cope with the immediate stressor. Once the threat subsides, cortisol levels return to normal.
In contrast, chronic stress, which involves long-term exposure to stressors without sufficient recovery periods, can result in sustained elevations in cortisol levels.
This chronic elevation can disrupt the normal functioning of the HPA axis and lead to various physiological and psychological consequences.
The effects of chronic stress on cortisol levels can contribute to the development of stress-related disorders and have long-lasting impacts on health.
Understanding the relationship between cortisol and stress, the effects of chronic stress on cortisol levels, and the role of CRH and ACTH in cortisol regulation provides insights into the complex interplay between stress and the body's physiological responses.
Managing stress effectively and implementing stress-reduction strategies can help maintain a healthy balance in cortisol levels and promote overall well-being.
Disorders of Cortisol Production
Addison's disease
Adrenal insufficiency, also known as Addison's disease, is a disorder characterized by insufficient production of cortisol and often aldosterone by the adrenal glands. This condition can be primary or secondary.
Primary adrenal insufficiency occurs when the adrenal glands are damaged or destroyed, often due to an autoimmune reaction.
Secondary adrenal insufficiency occurs when there is a dysfunction in the pituitary gland or hypothalamus, resulting in reduced production of ACTH.
Symptoms of adrenal insufficiency can vary but commonly include fatigue, weight loss, muscle weakness, low blood pressure, salt cravings, and skin darkening.
Individuals with adrenal insufficiency are at risk of adrenal crisis, a life-threatening condition characterized by severe symptoms, such as abdominal pain, vomiting, dehydration, low blood sugar, and confusion.
Treatment for adrenal insufficiency typically involves hormone replacement therapy with cortisol and sometimes aldosterone to restore normal hormone levels and manage symptoms.
Cushing's Syndrome
Cushing's syndrome is characterized by too much cortisol in the body. Various factors, including prolonged use of corticosteroid medications or hormonal imbalances, can cause it.
The most common cause is corticosteroid medications, often prescribed to manage asthma, rheumatoid arthritis, and autoimmune disorders.
However, Cushing's syndrome can also occur due to overactive adrenal glands or a pituitary tumor that produces excess ACTH.
Symptoms of Cushing's syndrome can include weight gain, particularly in the face and abdomen, muscle weakness, thinning skin, easy bruising, high blood pressure, and increased susceptibility to infections.
Treatment options for Cushing's syndrome depend on the underlying cause and may include surgery to remove tumors, medication adjustments, or other interventions to normalize cortisol levels.
Pituitary Tumors and ACTH Production
Pituitary tumors can disrupt the normal regulation of cortisol production by affecting the production and release of ACTH.
This results in the symptoms and complications associated with Cushing's syndrome. On the other hand, tumors in the pituitary gland that affect the normal production of ACTH can cause decreased ACTH levels and, subsequently, adrenal insufficiency, leading to decreased cortisol production
The diagnosis and management of pituitary tumors involving cortisol regulation typically involve a combination of imaging studies, hormone level measurements, and other specialized tests.
Treatment options depend on the specific type and size of the tumor and may include surgery, radiation therapy, medication, or a combination of these approaches.
Measuring Cortisol Levels
Cortisol levels in the body can be assessed through urine and blood tests.
- Urine tests: Cortisol urine tests involve collecting a 24-hour urine sample, which is then analyzed to measure the total amount of cortisol excreted. This test evaluates cortisol production over a longer period, helping to assess overall cortisol output.
- Blood tests: these tests are another method to measure cortisol levels. The morning cortisol level measurement involves obtaining a blood sample when cortisol levels are typically at their highest. This test can help diagnose conditions such as Cushing's syndrome or adrenal insufficiency.
- Suppression tests: The dexamethasone suppression test is another blood test that evaluates how the body responds to the synthetic corticosteroid dexamethasone. It helps differentiate between causes of cortisol dysregulation.
Cortisol urine and blood tests are valuable tools for diagnosing and monitoring cortisol production and regulation disorders.
They provide important information about cortisol levels, aiding healthcare professionals in determining appropriate treatment approaches and evaluating the effectiveness of interventions.
Frequently Asked Questions About Cortisol
What are the effects of chronic stress on cortisol levels?
Chronic stress can lead to elevated levels of cortisol in the body.
When the body perceives a threat or experiences prolonged stressful situations, the hypothalamus in the brain releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to release adrenocorticotropic hormone (ACTH).
ACTH, in turn, stimulates the adrenal glands to release cortisol. With chronic stress, this process can become dysregulated, resulting in chronically high cortisol levels, which can have detrimental effects on various organ systems in the body.
What are the common disorders associated with cortisol production?
Disorders associated with cortisol production include:
- Adrenal insufficiency
- Cushing's syndrome,
- Pituitary tumors affecting ACTH production.
In adrenal insufficiency, cortisol production is insufficient, whereas, in Cushing's syndrome, cortisol production is excessive. Pituitary tumors can increase or decrease ACTH production, resulting in abnormal cortisol levels.
References
Physiology, Cortisol - StatPearls
Cortisol Effects on Body Mass, Blood Pressure, and Cholesterol in the General Population - AHA
Cushing Disease / Cushing Syndrome - OHSU
Addison's disease - Mayo Clinic
Disclaimer
The contents of this article are provided for informational purposes only and are not intended to substitute for professional medical advice, diagnosis, or treatment. It is always recommended to consult with a qualified healthcare provider before making any health-related changes or if you have any questions or concerns about your health. Anahana is not liable for any errors, omissions, or consequences that may occur from using the information provided.

By: Emma Lee
Emma is an editor for Anahana and a soon-to-be graduate of the Master of Science program at the University of Toronto. She graduated with a Bachelor’s in Neuroscience and Immunology at the University of Toronto and has extensive experience in research. She is passionate about learning the science behind health and wellness and hopes to contribute her knowledge to help people live healthier lives. Outside of Anahana, Emma enjoys exploring nature, playing with her dog, and doing arts and crafts.